TL;DR
Over 7.5 Million Britons Face Record NHS Waiting Lists Uncover How Private Health Insurance Provides Rapid Access to Diagnostics, Specialist Treatment, and Peace of Mind, Shielding Your Health, Wealth, and Quality of Life from Unacceptable Delays The figures are staggering, and for millions across the UK, they represent a daily reality of pain, anxiety, and uncertainty. As of early 2025, the NHS waiting list for elective treatment in England has swollen to over 7.5 million referrals. This isn't just a statistic; it's a queue of people—parents, employees, retirees—waiting for procedures like hip replacements, cataract surgery, and vital diagnostic scans.
Key takeaways
- Total Waiting List: The referral-to-treatment (RTT) waiting list in England consistently hovers above 7.5 million. This represents millions of individual treatment pathways, not unique patients, but signifies a monumental backlog.
- Long Waits Persist: Despite efforts to clear the backlog, an estimated 350,000-400,000 people have been waiting for more than 52 weeks (one year) for their treatment to begin.
- The "Hidden" Backlog: Official figures don't always capture the full story. There are significant "hidden" waiting lists for crucial diagnostic tests. Projections suggest over 1.6 million people are waiting for key tests like MRI scans, CT scans, endoscopies, and ultrasounds. This initial delay creates a bottleneck that pushes back consultations and eventual treatment even further.
- Regional Disparities: Your postcode can drastically affect your wait time. Certain NHS trusts, particularly in densely populated or under-resourced areas, face much longer lists than others.
- Cancer Treatment Targets: While urgent cancer referrals are prioritised, the strain on diagnostics and staff means that crucial targets, such as starting treatment within 62 days of an urgent GP referral, are frequently being missed across the country.
Over 7.5 Million Britons Face Record NHS Waiting Lists Uncover How Private Health Insurance Provides Rapid Access to Diagnostics, Specialist Treatment, and Peace of Mind, Shielding Your Health, Wealth, and Quality of Life from Unacceptable Delays
The figures are staggering, and for millions across the UK, they represent a daily reality of pain, anxiety, and uncertainty. As of early 2025, the NHS waiting list for elective treatment in England has swollen to over 7.5 million referrals. This isn't just a statistic; it's a queue of people—parents, employees, retirees—waiting for procedures like hip replacements, cataract surgery, and vital diagnostic scans. For many, the wait stretches beyond the 18-week target, with hundreds of thousands waiting over a year for care.
This unprecedented pressure on our cherished National Health Service means that a treatable condition can escalate, impacting not just your physical health but your ability to work, your financial stability, and your overall quality of life. The prolonged discomfort and mental anguish of being "in limbo" can be as debilitating as the condition itself.
But what if there was a way to bypass the queue? What if you could see a specialist in days, not months, and receive treatment within weeks? This is the powerful proposition of Private Medical Insurance (PMI). Once seen as a luxury, PMI is now becoming a pragmatic and essential tool for individuals and families seeking to regain control over their health and wellbeing.
This comprehensive guide will unpack the reality of the NHS waiting list crisis and provide a definitive overview of how private health insurance works as a robust solution. We will explore its benefits, what it covers, how much it costs, and how you can choose a policy that shields you and your loved ones from the unacceptable cost of delay.
The NHS Waiting List Crisis: A Closer Look at the 2025 Figures
To understand the value of private healthcare, we must first grasp the scale of the challenge facing the NHS. The numbers paint a stark picture of a system stretched to its limits.
- Total Waiting List: The referral-to-treatment (RTT) waiting list in England consistently hovers above 7.5 million. This represents millions of individual treatment pathways, not unique patients, but signifies a monumental backlog.
- Long Waits Persist: Despite efforts to clear the backlog, an estimated 350,000-400,000 people have been waiting for more than 52 weeks (one year) for their treatment to begin.
- The "Hidden" Backlog: Official figures don't always capture the full story. There are significant "hidden" waiting lists for crucial diagnostic tests. Projections suggest over 1.6 million people are waiting for key tests like MRI scans, CT scans, endoscopies, and ultrasounds. This initial delay creates a bottleneck that pushes back consultations and eventual treatment even further.
- Regional Disparities: Your postcode can drastically affect your wait time. Certain NHS trusts, particularly in densely populated or under-resourced areas, face much longer lists than others.
- Cancer Treatment Targets: While urgent cancer referrals are prioritised, the strain on diagnostics and staff means that crucial targets, such as starting treatment within 62 days of an urgent GP referral, are frequently being missed across the country.
Why Are the Waiting Lists So Long?
This crisis is the result of a "perfect storm" of factors that have been brewing for years and were supercharged by the COVID-19 pandemic:
- Pandemic Legacy: Halting non-urgent elective care during the pandemic created an immense backlog that the system is still struggling to clear.
- Staffing Shortages: The NHS is facing a chronic shortage of doctors, nurses, and specialist staff, exacerbated by burnout and industrial action over pay and conditions.
- Growing and Ageing Population: An older population naturally requires more healthcare, placing increasing demand on services from joint replacements to cardiac care.
- Underfunding: While NHS funding has increased, many argue it hasn't kept pace with rising demand and inflation, impacting capacity for beds, equipment, and staff.
This combination of factors means that, for the foreseeable future, long waits for non-urgent care are set to remain a defining feature of the UK's health landscape.
| NHS Waiting List Metric | 2019 (Pre-Pandemic) | 2025 (Projected) | Impact on Patients |
|---|---|---|---|
| Total RTT Waiting List | ~4.4 million | ~7.6 million | Longer overall wait from referral |
| Patients Waiting > 52 Weeks | ~1,600 | ~380,000 | Extreme delays, health deterioration |
| Median Wait Time | ~8 weeks | ~14 weeks | Nearly doubled time in uncertainty |
| Diagnostic Test Waits | Variable | Up to 12 weeks+ | Delays diagnosis, anxiety |
The True Cost of Waiting: Health, Wealth, and Wellbeing
Waiting for healthcare isn't a passive activity; it carries a significant and multi-faceted cost that erodes your quality of life.
The Health Cost
For many conditions, time is critical. A delay in treatment can have severe clinical consequences:
- Condition Deterioration: A painful hip or knee can lead to reduced mobility, muscle wastage, and increased strain on other joints.
- Acute Becomes Chronic: A treatable acute issue, if left long enough, can become a chronic pain condition that is much harder to manage.
- Increased Complexity: A delayed diagnosis or treatment can make the eventual surgery or procedure more complex, potentially leading to longer recovery times.
- Mental Health Impact: The constant pain, uncertainty, and feeling of helplessness are major contributors to anxiety and depression, compounding the physical health problem.
Consider this example: A 55-year-old teacher with severe cataracts. The NHS wait for surgery is 12 months. During this time, her vision deteriorates to the point where she can no longer drive, read comfortably, or mark students' work effectively. Her independence is curtailed, and her ability to do her job is compromised, all while waiting for a routine, 20-minute procedure.
The Financial Cost
The link between health and wealth has never been clearer. The Office for National Statistics (ONS) has consistently reported a rise in economic inactivity due to long-term sickness. Waiting for NHS treatment is a key driver of this trend.
- Loss of Income: If your condition prevents you from working, you face a significant loss of earnings. Statutory Sick Pay is minimal, and not everyone has generous company sick pay policies.
- Career Stagnation: You may have to turn down promotions, reduce your hours, or even leave your job entirely.
- Impact on Self-Employed: For freelancers, contractors, and business owners, the impact is immediate and direct. If you can't work, you don't get paid.
This financial strain adds immense stress at a time when you are already vulnerable, creating a vicious cycle of poor health and financial worry.
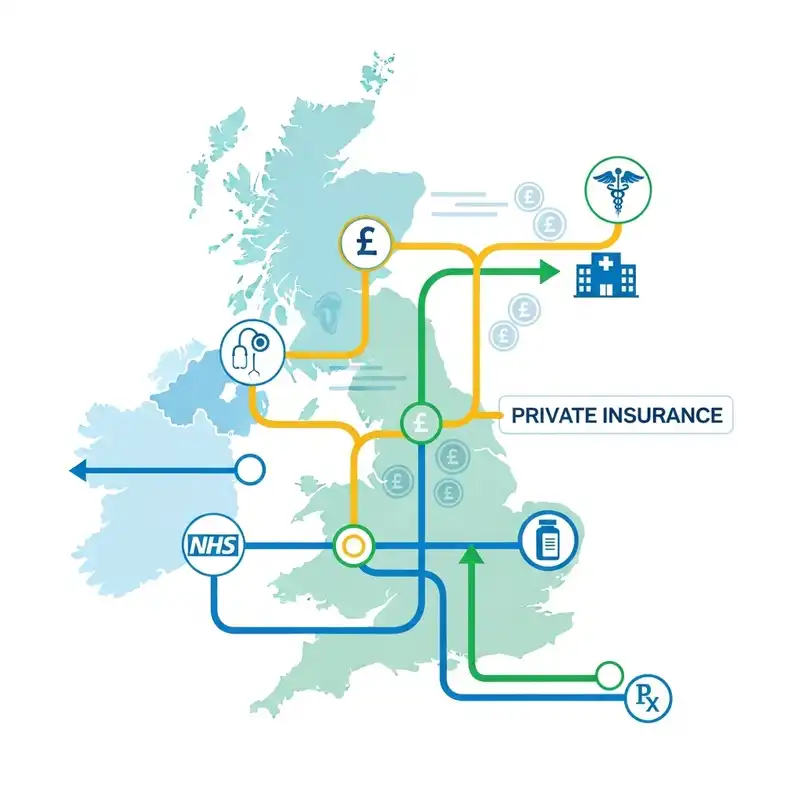
What is Private Medical Insurance (PMI) and How Does It Work?
Private Medical Insurance is a policy you pay for—typically via a monthly or annual premium—that covers the cost of private medical care for eligible conditions. In essence, it provides a parallel pathway to the NHS, giving you access to private hospitals, specialists, and diagnostic facilities.
The core purpose of PMI is to diagnose and treat acute conditions that arise after you have taken out your policy.
The Most Important Rule: Acute vs. Chronic and Pre-existing Conditions
This is the single most important concept to understand about standard PMI in the UK. Failure to grasp this can lead to disappointment and frustration.
- Acute Condition: A disease, illness, or injury that is likely to respond quickly to treatment and lead to a full recovery. Examples include joint replacements, hernia repair, cataract surgery, removing gallstones, or treating most cancers. PMI is designed for these.
- Chronic Condition: A disease, illness, or injury that has one or more of the following characteristics: it needs long-term monitoring, is incurable, has recurring symptoms, or requires ongoing management. Examples include diabetes, hypertension, asthma, arthritis, and multiple sclerosis. Standard PMI does NOT cover the long-term management of chronic conditions.
- Pre-existing Condition: Any condition for which you have experienced symptoms, received medication, or sought advice in a set period (usually 5 years) before your policy began. Standard PMI does NOT cover pre-existing conditions.
PMI is not a replacement for the NHS. It works alongside it. You will still rely on the NHS for accident and emergency services, GP visits (unless your policy includes a private GP service), and the management of any chronic conditions.
The Patient Journey with PMI: A Step-by-Step Guide
So, how do you actually use your insurance? The process is refreshingly straightforward.
- Visit Your GP: Your journey almost always starts with your NHS GP. You discuss your symptoms, and if they feel you need to see a specialist, they will provide you with an open referral letter.
- Contact Your Insurer: You call your PMI provider's dedicated claims line, explain the situation, and provide the details from the GP referral.
- Claim Authorisation: The insurer checks that your condition is covered under the terms of your policy and authorises the claim, giving you a pre-authorisation number.
- Choose Your Specialist and Hospital: Your insurer will provide you with a list of approved specialists and high-quality private hospitals from their network. You have the choice of who you see and where you are treated.
- Book Your Appointments: You can now book your consultation, diagnostic scans, and subsequent treatment at a time and location that is convenient for you.
- Receive Treatment: You receive your care in a comfortable private facility, often with a private room, en-suite bathroom, and more flexible visiting hours.
- Bills Are Settled: The private hospital and specialist bill your insurance company directly. Apart from any excess you may have on your policy, you have nothing to pay.
The Core Benefits of PMI: Speed, Choice, and Comfort
The advantages of having a PMI policy can be summarised in three key areas that directly address the shortcomings of an overstretched public system.
1. Rapid Access to Diagnostics and Treatment
This is the primary reason people buy health insurance. The ability to bypass the queue is the most tangible benefit.
| Procedure/Scan | Typical NHS Wait Time (2025) | Typical Private Wait Time (with PMI) |
|---|---|---|
| MRI / CT Scan | 4 - 12 weeks | 3 - 7 days |
| Specialist Consultation | 4 - 10 months | 1 - 3 weeks |
| Hip / Knee Replacement | 12 - 18 months+ | 4 - 6 weeks |
| Cataract Surgery | 9 - 12 months | 3 - 5 weeks |
| Hernia Repair | 6 - 11 months | 2 - 4 weeks |
Disclaimer: Wait times are illustrative and can vary based on location, specialty, and the specific NHS Trust or private provider.
2. Unparalleled Choice and Control
The NHS is a fantastic service, but it is largely a "you get what you're given" system. PMI puts you back in the driver's seat.
- Choice of Consultant: You can research and choose a leading specialist in their field.
- Choice of Hospital: Insurers have extensive networks of high-quality private hospitals across the UK, allowing you to choose one that is convenient or has a reputation for excellence in a particular area.
- Choice of Timing: You can schedule your surgery around your work commitments or family life, such as during school holidays, rather than accepting the first date you are offered.
3. Enhanced Comfort and Privacy
While clinical outcomes are paramount, the environment in which you recover plays a huge role in your wellbeing. Private hospitals typically offer:
- A private room with an en-suite bathroom.
- Unrestricted visiting hours for family and friends.
- A la carte menus and better quality food.
- Free TV, Wi-Fi, and other personal comforts.
This creates a calmer, more restful environment conducive to a faster and more pleasant recovery.
What Does Private Health Insurance Typically Cover? (And What Does It Exclude?)
Understanding the scope of your cover is vital. Policies are usually structured with a core offering and optional extras, allowing you to tailor the plan to your needs and budget.
What's Usually Covered
| Feature | Description |
|---|---|
| In-patient & Day-patient Care | Covers surgery costs, hospital accommodation, and specialist fees when you are admitted to a hospital bed, even for a day. This is the heart of every policy. |
| Comprehensive Cancer Cover | A standout feature. Often covers diagnosis, surgery, chemotherapy, radiotherapy, and even experimental drugs not yet available on the NHS. |
| Diagnostic Scans | Covers the cost of MRI, CT, and PET scans when part of in-patient or day-patient care. |
| Specialist Consultations | Covers the fees for seeing a consultant before and after your hospital treatment. |
Popular Optional Add-ons
| Feature | Description |
|---|---|
| Out-patient Cover | Essential for rapid diagnosis. Covers specialist consultations and diagnostic tests before you are admitted to hospital. Policies often have a limit (e.g., £1,000 per year or 2-3 consultations). |
| Mental Health Cover | Provides access to psychiatrists, psychologists, and therapists. Hugely valuable given the long NHS waits for mental health services. |
| Therapies Cover | Covers treatments like physiotherapy, osteopathy, and chiropractic care, often with a set number of sessions per year. |
| Dental & Optical Cover | Can contribute towards routine check-ups, emergency dental work, and the cost of glasses or contact lenses. |
What's Almost Always Excluded
It's equally important to know what PMI is not for.
- Pre-existing conditions (as explained earlier).
- Chronic conditions (like diabetes, asthma, hypertension). Your policy may cover the initial diagnosis, but the long-term management will revert to the NHS.
- Accidents & Emergencies. If you have a heart attack or are in a car accident, you go to your local A&E.
- Normal pregnancy and childbirth.
- Cosmetic surgery (unless it's for reconstruction after an accident or eligible surgery like a mastectomy).
- Organ transplants.
- Drug and alcohol abuse treatment.
Understanding the Cost of Private Health Insurance
There is no single price for PMI. Your premium is personal to you and is calculated based on several key factors.
- Age: This is the most significant factor. The older you are, the higher the statistical likelihood of claiming, so the premium will be higher.
- Location: Living in or near major cities, especially London, means access to more expensive hospitals, which increases the premium.
- Level of Cover: A basic policy covering only in-patient care will be much cheaper than a comprehensive plan with full out-patient, mental health, and therapies cover.
- Excess (illustrative): This is the amount you agree to pay towards a claim (e.g., the first £250). A higher excess will lower your monthly premium.
- Hospital List: Insurers offer different tiers of hospital access. A plan with a limited local network will be cheaper than one offering access to all hospitals nationwide, including premium Central London facilities.
- Underwriting Type: The method the insurer uses to assess your medical history can affect the price.
- No-Claims Discount: Similar to car insurance, you can build up a discount for every year you don't make a claim.
To give you a clearer idea, here are some illustrative monthly premiums.
| Profile | Basic Cover (Core only, £500 excess) | Comprehensive Cover (Full out-patient, £250 excess) |
|---|---|---|
| 30-year-old individual | £35 - £50 | £60 - £85 |
| 45-year-old individual | £55 - £75 | £90 - £130 |
| Couple, both aged 50 | £120 - £160 | £200 - £280 |
| Family (2 adults, 2 kids) | £150 - £200 | £250 - £350 |
These are estimates for non-smokers outside London. Prices vary significantly between insurers.
Navigating these options to find the best value can be daunting. At WeCovr, we specialise in this. Our expert advisors compare plans and prices from all the UK's leading insurers, including Bupa, AXA Health, Aviva, and Vitality, to find a policy that perfectly matches your needs and budget.
How to Choose the Right PMI Policy for You
Making the right choice requires careful consideration of your personal circumstances. Here is a structured approach.
Step 1: Assess Your Needs and Budget
Think about why you want the cover. Are you primarily concerned about long waits for surgery? Or is rapid diagnosis via out-patient cover your priority? Do you have a family history of cancer or heart conditions? Be realistic about what you can afford each month.
Step 2: Understand Underwriting Options
This is a crucial technical choice that determines how the insurer treats your past medical conditions.
- Moratorium (Most Common): You don't declare your full medical history upfront. Instead, the policy automatically excludes any condition you've had symptoms of or treatment for in the last 5 years. However, if you remain treatment- and symptom-free for that condition for a continuous 2-year period after your policy starts, the insurer may then cover it. It's simpler but less certain.
- Full Medical Underwriting (FMU): You complete a detailed health questionnaire. The insurer assesses your history and tells you upfront exactly what is excluded from cover, permanently. This provides absolute clarity from day one but requires more initial paperwork.
Step 3: Select Your Policy Options
- Decide on Out-patient Cover: For most people, some level of out-patient cover is highly recommended as it speeds up the entire diagnostic process.
- Consider a 6-Week Option: A popular way to reduce costs. This clause means your policy will only cover your treatment if the NHS wait for it is longer than six weeks. If the NHS can treat you within six weeks, you use the NHS. This can significantly lower your premium.
- Choose Your Hospital List: If you live outside a major city and are happy to be treated locally, choosing a more restricted hospital list can save you money.
Step 4: Use an Independent, Expert Broker
The UK health insurance market is complex, with dozens of providers and hundreds of policy combinations. This is where an independent broker like WeCovr is invaluable. We are not tied to any single insurer. Our sole objective is to find the best possible cover for you.
We cut through the jargon, compare the small print, and leverage our industry knowledge to find the right balance of cover and cost. We ensure you understand exactly what you are buying, so there are no nasty surprises if you need to claim. As an added benefit, because we care about our customers' holistic wellbeing, we provide all our clients with complimentary access to our AI-powered nutrition and calorie tracking app, CalorieHero, empowering you to take proactive steps towards a healthier lifestyle.
Real-Life Scenarios: How PMI Works in Practice
Let's look at how a policy could help in real situations.
Case Study 1: Mark, the Self-Employed Builder Mark, 52, develops chronic hip pain. His GP suspects osteoarthritis and refers him to an orthopaedic specialist. The NHS wait for a consultation is 9 months, with a potential 18-month wait for a hip replacement. Unable to work and losing income daily, Mark uses his PMI policy.
- Week 1: Calls his insurer, gets authorisation, and books a private consultation.
- Week 2: Sees a top surgeon who confirms he needs a hip replacement. An MRI is done the next day.
- Week 5: Undergoes surgery in a comfortable private hospital.
- 3 Months Later: After intensive physiotherapy (also covered by his policy), Mark is back at work, earning again.
PMI's Impact: Mark avoided almost two years of pain and lost income. The policy effectively paid for itself many times over.
Case Study 2: David, the Cancer Diagnosis David, 62, is diagnosed with early-stage prostate cancer following a GP check-up. While the NHS offers excellent cancer care, his comprehensive PMI policy provides additional options and speed.
- Speed: He sees a leading oncologist within a week.
- Advanced Diagnostics: His policy covers a state-of-the-art PSMA PET scan, which provides a more precise picture of the cancer's location, helping to tailor the treatment.
- Choice of Treatment: He is offered a choice between traditional surgery, radiotherapy, and minimally invasive robotic surgery (da Vinci), which is less widely available on the NHS and offers a faster recovery with fewer side effects.
- Comfort: He receives chemotherapy in a quiet, private suite rather than a busy ward.
PMI's Impact: David benefited from speed, cutting-edge technology, and choice, giving him enormous peace of mind and control during a frightening time.
Taking Control of Your Health in Uncertain Times
The NHS remains one of our nation's greatest assets, and its emergency and critical care services are world-class. However, for elective procedures and diagnostics, the system is facing a crisis of capacity that will not be resolved overnight.
Waiting months or years for treatment is no longer a minor inconvenience; it is a major threat to our health, finances, and quality of life. Private Medical Insurance has transformed from a "nice-to-have" perk into an essential part of a modern financial and health planning toolkit. It offers a direct, effective, and accessible way to bypass the queues, providing rapid access to high-quality care when you need it most.
By investing in a PMI policy, you are not turning your back on the NHS. You are making a sensible, proactive choice to protect yourself and your family. You are buying certainty in uncertain times. You are buying peace of mind.
Don't let your health become a number on a waiting list. Explore your options, understand the benefits, and take the first step towards securing fast, effective healthcare.
Ready to take control? Speak to a friendly, expert advisor at WeCovr today for a free, no-obligation quote and discover how affordable your peace of mind can be.
Sources
- NHS England: Waiting times and referral-to-treatment statistics.
- Office for National Statistics (ONS): Health, mortality, and workforce data.
- NICE: Clinical guidance and technology appraisals.
- Care Quality Commission (CQC): Provider quality and inspection reports.
- UK Health Security Agency (UKHSA): Public health surveillance reports.
- Association of British Insurers (ABI): Health and protection market publications.