Fast Track to Gut Health How UK Private Health Insurance Covers Digestive Issues

Fast Track to Gut Health: How UK Private Health Insurance Covers Digestive Issues
Digestive health is the cornerstone of overall well-being, yet for millions in the UK, issues ranging from discomfort to chronic conditions can severely impact daily life. From the pervasive rumble of IBS to the debilitating pain of Crohn's disease or diverticulitis, gut problems are not just an inconvenience; they can be profoundly life-altering. In an era where understanding of the gut microbiome and its far-reaching effects is rapidly advancing, access to timely and effective care is more crucial than ever.
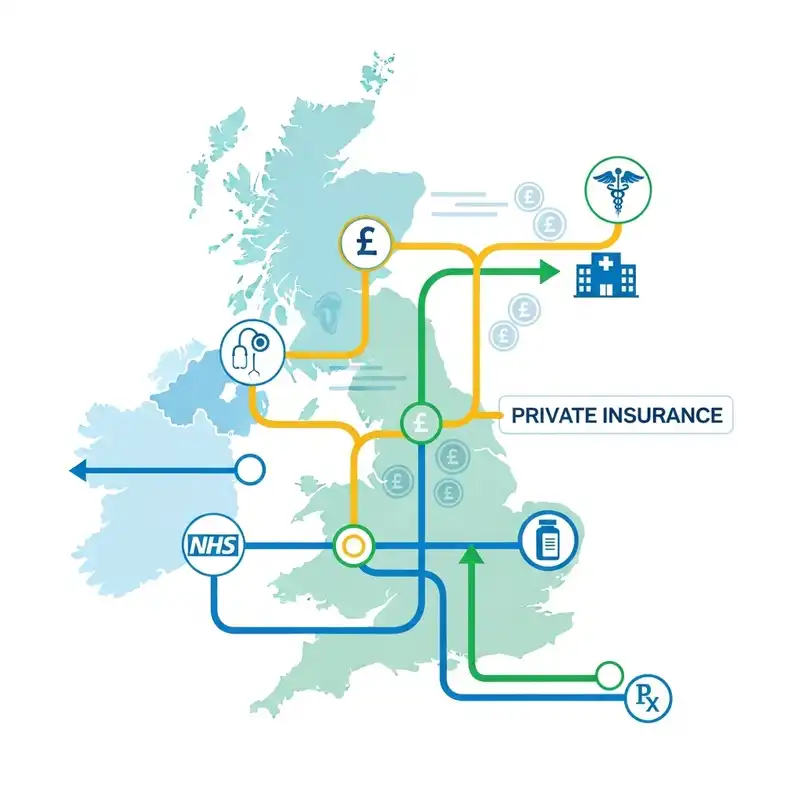
While the NHS provides outstanding care, the increasing demand often leads to lengthy waiting lists for diagnostic tests, specialist consultations, and treatments. This can be particularly distressing when dealing with sensitive and often painful digestive symptoms that require prompt investigation. This is where UK private health insurance (PMI) can offer a lifeline, providing a potential "fast track" to diagnosis and treatment for acute digestive issues.
This comprehensive guide will delve into how UK private health insurance works in the context of digestive health, what it typically covers, its limitations (especially regarding pre-existing and chronic conditions), and how you can navigate this complex landscape to secure peace of mind.
Understanding the Gut-Health Landscape in the UK
Digestive health issues are incredibly prevalent across the UK. Conditions like Irritable Bowel Syndrome (IBS), gastro-oesophageal reflux disease (GERD), coeliac disease, diverticular disease, and inflammatory bowel diseases (IBD) such as Crohn's disease and Ulcerative Colitis affect a significant portion of the population.
The symptoms can range from mild bloating and indigestion to severe abdominal pain, chronic diarrhoea, bleeding, and weight loss. These symptoms not only cause physical discomfort but can also lead to significant anxiety, depression, and a reduced quality of life, impacting work, social activities, and personal relationships.
For many, the initial step is a visit to their GP, who can offer initial advice and potentially prescribe medication. However, if symptoms persist or are severe, further investigation by a gastroenterologist – a specialist in digestive health – becomes necessary. Waiting times for these specialist referrals and subsequent diagnostic tests (like endoscopies or colonoscopies) on the NHS can stretch into weeks or even months, a period of uncertainty that can be emotionally and physically taxing for those experiencing distressing symptoms.
The Impact of Delays
Delays in diagnosis can lead to:
- Prolonged suffering: Unaddressed symptoms continue to cause discomfort and distress.
- Worsening conditions: Some conditions can progress if not diagnosed and treated promptly.
- Increased anxiety: Uncertainty about symptoms can significantly impact mental health.
- Disruption to daily life: Persistent symptoms can hinder work, education, and social engagement.
This is precisely where private health insurance presents a compelling alternative, offering an expedited pathway to expert medical opinion and necessary interventions, for new and acute conditions.
What is Private Health Insurance and How Does it Work?
Private health insurance, often referred to as Private Medical Insurance (PMI), is a policy that covers the cost of private healthcare treatments for acute medical conditions that arise after you’ve taken out the policy. It works alongside the NHS, offering you choices and faster access to care.
Core Benefits of PMI for Digestive Issues (and general health)
- Faster Access: Significantly reduced waiting times for consultations, diagnostic tests, and treatments.
- Choice of Specialist: The ability to choose your consultant and often the hospital where you receive treatment.
- Comfort and Privacy: Treatment in private hospitals or private wings of NHS hospitals, offering private rooms, flexible visiting hours, and improved amenities.
- Flexible Appointments: Greater flexibility in scheduling appointments to suit your lifestyle.
- Access to New Treatments: Potentially access to drugs and treatments not yet routinely available on the NHS (though this varies by policy and insurer).
How Policies are Underwritten: Understanding Your Coverage
When you apply for private health insurance, the insurer needs to assess your medical history to determine what they will and won't cover. This process is called 'underwriting'. There are two main types of underwriting in the UK:
1. Full Medical Underwriting (FMU)
With FMU, you provide a comprehensive medical history when you apply. You'll typically fill out a detailed health questionnaire covering your past and present conditions, consultations, and treatments. The insurer then assesses this information.
- Pros: You know upfront exactly what is covered and, more importantly, what is excluded based on your medical history. This provides clarity from the start.
- Cons: The application process can take longer due to the detailed medical review.
For any pre-existing conditions disclosed during FMU, the insurer will make an explicit decision:
- Covered: In very rare cases, if a condition was minor and fully resolved a long time ago, they might offer to cover it.
- Excluded: This is the most common outcome for pre-existing conditions, meaning any future treatment related to that condition will not be covered. This exclusion will be clearly stated in your policy documents.
- Moratorium Applied: In some cases, for conditions that haven't caused symptoms for a certain period (e.g., 2 years), they might be covered after a 'moratorium' period, provided you have no symptoms or treatment for them during that time.
2. Moratorium Underwriting
This is often the most common and quicker way to get cover. With moratorium underwriting, you don't typically need to fill out a detailed medical questionnaire upfront. Instead, the insurer automatically excludes any medical condition you've had symptoms, advice, or treatment for during a specific period before you take out the policy (e.g., the last 5 years). This is known as the 'moratorium period' (usually 2 years from the start of your policy).
- How it works: If you have no symptoms, advice, or treatment for a pre-existing condition during the 2-year moratorium period, that condition may become eligible for cover after this period. However, if you have a flare-up or need treatment for it during the moratorium, the 2-year period effectively "resets" for that specific condition.
- Pros: It's a faster and simpler application process.
- Cons: You won't know exactly what's covered or excluded until you make a claim. This can lead to uncertainty and potential disappointment if a claim for a previously dormant condition is denied.
Crucial Point on Pre-Existing and Chronic Conditions:
Regardless of the underwriting type, private health insurance generally does not cover pre-existing conditions. A pre-existing condition is typically defined as any disease, illness, or injury for which you have received medication, advice, or treatment, or had symptoms, before the start date of your insurance policy.
Furthermore, private health insurance is designed to cover acute conditions, not chronic ones. An acute condition is an illness, injury, or disease that is likely to respond quickly to treatment, or that is short-lived. A chronic condition is an illness, injury, or disease that has one or more of the following characteristics:
- It needs long-term ongoing care or supervision.
- It comes back or is likely to come back.
- It requires a long period of observation.
- It has no known cure.
- It is permanent.
This means conditions like Irritable Bowel Syndrome (IBS), Crohn's disease, Ulcerative Colitis, or chronic GERD, once diagnosed and managed long-term, are typically considered chronic. While private health insurance might cover the initial diagnosis of a new onset of these conditions, it generally will not cover ongoing management, flare-ups, or long-term medication for a condition that has already been diagnosed and is considered chronic or pre-existing. This distinction is paramount when considering PMI for digestive health.
Navigating Digestive Concerns: How PMI Steps In
When you experience new, acute digestive symptoms, private health insurance can provide a vital pathway to swift diagnosis and treatment.
The Private Healthcare Pathway for Digestive Issues:
- GP Referral: Your journey typically begins with your NHS GP. They will assess your symptoms and, if appropriate, recommend a referral to a private gastroenterologist. Most insurers require a GP referral to authorise private treatment.
- Insurers Pre-Authorisation: Once you have a referral, you contact your insurer to "pre-authorise" the consultation and any initial diagnostic tests. This is a crucial step; always get pre-authorisation before incurring costs.
- Specialist Consultation: You can then book an appointment with your chosen private gastroenterologist, often within days.
- Diagnostic Procedures: If necessary, the specialist will recommend diagnostic tests, which can be arranged quickly.
- Treatment: Based on the diagnosis, the specialist will propose a treatment plan. If this involves surgery or specific medications for an acute condition, your insurer will typically cover the costs, subject to your policy terms.
Common Digestive Conditions and Procedures PMI May Cover (for acute onset and new conditions):
| Condition/Symptom Covered (if acute/new onset) | What PMI Can Typically Cover (Diagnostic & Acute Treatment) | What PMI Will NOT Cover (Typically) |
|---|---|---|
| New, unexplained abdominal pain | Consultations with gastroenterologist, blood tests, scans (ultrasound, CT, MRI), endoscopy, colonoscopy. | Pre-existing chronic abdominal pain (e.g., from diagnosed IBS). |
| New onset severe acid reflux/dyspepsia | Consultations, upper GI endoscopy, medication for acute relief. | Ongoing management of chronic GERD, repeat prescriptions for long-term use for a chronic condition. |
| New rectal bleeding | Consultations, colonoscopy, flexible sigmoidoscopy, treatment of acute haemorrhoids (e.g., banding). | Ongoing management of diagnosed Ulcerative Colitis or Crohn's disease related bleeding (chronic). |
| Sudden change in bowel habits (acute) | Consultations, stool tests, colonoscopy/endoscopy to rule out serious conditions. | Management of established IBS, chronic constipation/diarrhoea. |
| Gallstones (symptomatic) | Consultations, ultrasound, cholecystectomy (gallbladder removal surgery). | Asymptomatic gallstones, pre-existing history of gallstone attacks managed conservatively. |
| Diverticulitis (acute flare-up) | Consultations, CT scans, antibiotics, hospital admission for acute management. | Ongoing management of diverticular disease, preventing future flare-ups, dietary advice for chronic condition. |
| Appendicitis (acute) | Consultations, scans, appendicectomy (emergency surgery). | (Always an emergency, initially NHS, but PMI can cover transfer to private post-stabilisation if policy allows). |
| Hernias (e.g., inguinal, umbilical) | Consultations, physical examination, hernia repair surgery. | Pre-existing asymptomatic hernias unless specific criteria met (rare). |
This table provides general examples and is not exhaustive. Coverage always depends on your specific policy terms, level of cover, and underwriting agreement.
Diagnostic Procedures Commonly Covered:
- Endoscopy: Examination of the upper digestive tract (oesophagus, stomach, duodenum) using a thin, flexible tube with a camera.
- Colonoscopy: Examination of the large intestine (colon) and rectum.
- Flexible Sigmoidoscopy: Examination of the lower part of the colon.
- Capsule Endoscopy: Ingesting a small camera capsule to image the small intestine.
- Ultrasound Scans: To visualise organs like the gallbladder, liver, and pancreas.
- CT Scans: Detailed cross-sectional images of internal organs.
- MRI Scans: Advanced imaging for soft tissues, often used for inflammatory bowel disease assessment.
- Blood Tests: For inflammation markers, liver function, coeliac disease antibodies, etc.
- Stool Tests: To check for infections, blood, or inflammatory markers.
All these diagnostic steps are crucial for identifying the cause of new, acute digestive symptoms, and PMI can significantly reduce the waiting time to undergo them.
Beyond Basic Care: Enhancements and Ancillary Benefits
Some private health insurance policies, particularly more comprehensive ones, may offer benefits that extend beyond direct acute treatment. These can be valuable for holistic well-being, though their coverage for digestive issues might be indirect or limited.
- Mental Health Support: The gut-brain axis is a well-established connection. Stress and anxiety can significantly impact digestive health, and vice versa. Many policies now include cover for talking therapies (like CBT), counselling, or even psychiatric consultations, which can be invaluable for managing the psychological impact of chronic or undiagnosed digestive issues. This may not directly treat the gut, but it supports the individual coping with its symptoms.
- Physiotherapy/Osteopathy/Chiropractic: While not directly for gut health, some musculoskeletal issues can mimic or exacerbate abdominal pain (e.g., back pain referral). If these therapies are covered for a diagnosed condition, they could indirectly help alleviate some discomfort.
- Dietetic Consultations: Some higher-tier policies might offer a limited number of consultations with a registered dietitian, if referred by a specialist for an acute, covered condition. This can be beneficial for understanding dietary triggers or management post-surgery, but typically won't cover long-term dietary counselling for chronic conditions like IBS unless explicitly specified as a benefit for a covered acute event.
- Health Assessments/Screening: While not typically included as part of standard acute medical insurance, some insurers offer optional health assessments or screening packages. These might include blood tests or health checks that could identify risk factors, but are generally preventative and separate from claims for specific symptoms.
- Wellness Programs: Some insurers offer digital tools, apps, or discounts on gym memberships/health products as part of broader wellness initiatives. These are generally not direct medical benefits but support a healthy lifestyle which can positively influence gut health.
It's vital to carefully review the policy terms and conditions for these ancillary benefits, as they often come with specific limitations, referral requirements, or are part of higher-premium plans.
The Exclusions: What Private Health Insurance Typically Doesn't Cover for Digestive Health
Understanding what isn't covered is just as important as understanding what is. Misconceptions about coverage, particularly concerning digestive health, are common.
1. Pre-existing Conditions
As discussed, this is the most significant exclusion. If you had symptoms, received advice, or had treatment for a digestive condition before your policy started, it will almost certainly be excluded. This includes:
- Established IBS: If you've been diagnosed with IBS for years, flare-ups or ongoing management will not be covered.
- Diagnosed Inflammatory Bowel Disease (Crohn's, Ulcerative Colitis): Once diagnosed, the ongoing management, medication, and flare-ups of these chronic conditions are excluded.
- Chronic Diverticular Disease: If you've had previous diverticulitis episodes, ongoing management or prevention is excluded.
- Long-standing GERD: If you've been managing reflux for a long time with medication or lifestyle changes, ongoing treatment won't be covered.
Example: If you suffered from acid reflux five years ago, received a diagnosis, and occasional medication from your GP, even if symptoms are currently mild, any future need for specialist investigation or treatment related to that reflux will be considered a pre-existing condition and excluded.
2. Chronic Conditions
Even if a chronic condition manifests after your policy starts, private health insurance typically only covers the initial diagnostic phase and acute treatment of its initial presentation. It does not cover the long-term management, monitoring, or treatment of chronic conditions.
Example: If you develop symptoms indicative of Crohn's disease after taking out your policy, your insurance might cover the initial consultations, diagnostic tests (e.g., colonoscopy, MRI), and potentially the initial acute treatment. However, once diagnosed as a chronic condition requiring ongoing medication and monitoring, subsequent treatment and flare-ups will usually revert to the NHS.
3. Emergency Treatment
Private health insurance is not a substitute for emergency services. If you experience a medical emergency, such as a severe acute appendicitis attack, sudden severe gastrointestinal bleeding requiring immediate attention, or a suspected perforated bowel, you should always go to an NHS Accident & Emergency (A&E) department or call 999. PMI does not cover A&E visits or emergency admissions, although some policies might cover transfer to a private hospital once stabilised, if medically appropriate and pre-authorised.
4. General Exclusions Applicable to All Conditions:
- Conditions related to drug or alcohol abuse.
- Cosmetic surgery or treatment.
- Fertility treatment.
- Routine maternity care.
- Experimental or unproven treatments.
- Overseas treatment (unless a specific travel add-on is purchased).
- Self-inflicted injuries.
- Treatment for HIV/AIDS.
- Organ transplants (with very few exceptions for specific organs on some high-tier policies).
- Treatment covered by the NHS (you cannot claim for treatment you receive on the NHS).
Table: Typical Exclusions for Digestive Health in PMI
| Category of Exclusion | Specific Digestive Examples | Why it's Excluded |
|---|---|---|
| Pre-existing Conditions | Long-standing IBS, previously diagnosed Crohn's/UC, chronic diverticular disease, pre-existing GERD. | PMI covers new, acute conditions, not those you've already had or been treated for. |
| Chronic Conditions (Ongoing Management) | Regular medication for Ulcerative Colitis, dietary management for diagnosed Coeliac Disease, ongoing pain management for chronic pancreatitis. | PMI aims to return you to health from an acute illness; it doesn't cover lifelong management of incurable conditions. |
| Emergency Treatment | Acute appendicitis requiring immediate surgery, severe internal bleeding requiring A&E admission. | These are best handled by NHS emergency services. |
| Screening/Preventative Care | Routine colon cancer screening without symptoms, general gut microbiome testing. | PMI typically covers treatment for diagnosed conditions, not general health screening or preventative tests unless specific add-ons are chosen. |
| Unproven/Experimental Treatment | Very niche or new gut therapies not recognised by mainstream medical bodies. | Insurers only cover treatments with established efficacy and safety profiles. |
| Travel-Related Incidents | Food poisoning contracted abroad. | Requires separate travel insurance. |
Understanding these exclusions is vital to manage your expectations and ensure you make an informed decision when purchasing private health insurance. Always read your policy documents carefully.
Choosing the Right Policy for Your Digestive Health Needs
Selecting the right private health insurance policy for digestive concerns requires careful consideration. It’s not a one-size-fits-all solution, and what suits one person may not suit another.
Here are the key factors to consider:
-
Level of Cover:
- In-patient Only: This is the most basic and cheapest option, covering only treatment that requires an overnight stay in hospital (e.g., surgery for gallstones). It typically excludes outpatient consultations and diagnostic tests.
- Out-patient Limits: Many policies offer a combined in-patient and out-patient cover, but with limits on how much they will pay for out-patient consultations, scans, and tests. For digestive issues where diagnosis often relies heavily on specialist consultations and tests, a decent outpatient limit is crucial.
- Comprehensive: This is the highest level of cover, offering generous or unlimited out-patient benefits, a wider choice of hospitals, and sometimes additional benefits like mental health support or therapies.
-
Excess: This is the amount you agree to pay towards the cost of your treatment before the insurer pays the rest. A higher excess usually means a lower monthly premium. Consider what you can comfortably afford if you need to make a claim.
-
Hospital Network: Policies often come with a choice of hospital lists:
- Full National List: Access to virtually all private hospitals.
- Guided Option/Limited List: Access to a smaller, pre-selected network of hospitals, which can reduce premiums. Ensure this list includes hospitals and specialists convenient for you.
-
Underwriting Method: As discussed, decide between Full Medical Underwriting (FMU) for upfront clarity on exclusions, or Moratorium for a simpler application process but deferred clarity. If you have any significant medical history, FMU might offer more peace of mind.
-
Additional Benefits: If mental health support, dietetic consultations, or other ancillary services are important to you, check if these are included or available as add-ons.
-
Budget: Premiums vary significantly based on your age, location, chosen level of cover, excess, and health history. Get multiple quotes and compare them carefully.
-
Read the Small Print: Always, always read the policy terms and conditions thoroughly. Pay particular attention to definitions of "acute" and "chronic" conditions, and the specifics of pre-existing condition exclusions.
The Role of Your GP: The Gateway to Private Care
It’s crucial to reiterate that in the UK, your GP remains the primary gatekeeper to both NHS and private specialist care.
The process is typically as follows:
- Initial Consultation: You start by seeing your NHS GP for your digestive symptoms.
- Assessment and Referral: Your GP will assess your condition. If they believe you require specialist investigation or treatment beyond what they can provide, they can offer a referral.
- Choice of Referral: Your GP can write an 'open referral' to a gastroenterologist, or if you have a specific specialist in mind (perhaps recommended by a friend or online search), your GP can make a named referral.
- Insurers Pre-Authorisation: Before booking your private appointment, you must contact your private health insurer with your GP's referral letter. The insurer will review the referral, check it aligns with your policy terms, and provide 'pre-authorisation'. This step is non-negotiable; without it, you risk your claim being denied, leaving you liable for the full cost.
- Private Pathway Begins: Once pre-authorised, you can proceed to book your private specialist consultation and any subsequent tests or treatments.
This system ensures that medical necessity is assessed by a qualified primary care physician before specialist private care is accessed, preventing unnecessary or inappropriate claims.
Real-Life Scenarios: How PMI Can Help (and Where it Can't)
Let's illustrate the practical application and limitations of private health insurance for digestive issues with a few hypothetical scenarios.
Scenario 1: New Onset Severe Acid Reflux (Positive PMI Case)
- Situation: Sarah, 40, has never had digestive problems before. Suddenly, she develops severe heartburn, regurgitation, and difficulty swallowing. Her GP suspects GERD but wants further investigation to rule out more serious conditions.
- PMI Role: Sarah has a comprehensive private health insurance policy. Her GP provides a referral to a private gastroenterologist. Sarah contacts her insurer for pre-authorisation, which is granted. Within a week, she sees a top gastroenterologist, who recommends an urgent endoscopy. The endoscopy is performed a few days later, identifying severe oesophagitis. She is prescribed medication, and a follow-up is scheduled. The entire process, from GP visit to diagnosis and initial treatment, takes just over two weeks.
- Outcome: PMI covered all consultations, the endoscopy, and the initial acute medication. Had this been a very new, acute case of reflux caused by an infection or specific acute event, PMI would cover the treatment to resolve it. If it becomes a long-term, chronic condition, the ongoing management of the GERD would typically revert to the NHS after the initial acute phase of diagnosis and treatment is complete.
Scenario 2: Suddenly Worsening IBS Symptoms (Negative PMI Case)
- Situation: Mark, 35, was diagnosed with Irritable Bowel Syndrome (IBS) five years ago, before he took out his private health insurance policy. He has generally managed his symptoms well with diet and lifestyle. Recently, however, his symptoms have become significantly worse, more painful, and frequent. He consults his GP, hoping his private insurance will cover new investigations to understand why his IBS is worsening.
- PMI Role: Mark contacts his insurer with his GP's referral. However, because his IBS was diagnosed and managed before he took out his policy (pre-existing condition), and it's a chronic condition, the insurer declines cover for any investigations or treatments related to the IBS, even if symptoms are worsening.
- Outcome: Mark must rely on the NHS for further investigations or management of his worsening IBS. While his symptoms have worsened, the underlying condition remains pre-existing and chronic. This highlights the crucial distinction between new acute problems and flare-ups of chronic or pre-existing conditions.
Scenario 3: Investigation of New, Unexplained Abdominal Pain (Positive PMI Case)
- Situation: Emily, 50, develops persistent, vague abdominal pain that is new and not related to her diet. Her GP is concerned and wants to rule out serious issues like gallstones or something more significant.
- PMI Role: Emily, who took out her policy last year with no prior abdominal issues, gets a GP referral. Her insurer pre-authorises consultations and an ultrasound scan. The scan quickly reveals gallstones, which are causing the pain. The gastroenterologist recommends gallbladder removal (cholecystectomy). The insurer approves the surgery, and Emily has the procedure in a private hospital within three weeks.
- Outcome: PMI covered all diagnostic steps and the acute surgical treatment, providing a rapid resolution to a new and distressing problem. The gallstones were a new, acute condition that developed after her policy started.
Scenario 4: Long-term Management of Diagnosed Ulcerative Colitis (Negative PMI Case)
- Situation: David, 28, was diagnosed with Ulcerative Colitis (UC) two years ago, a year after taking out his private health insurance. His initial diagnosis and acute treatment were covered by his PMI. He is now on long-term medication to manage his UC, but has occasional flare-ups. He wants his private insurance to cover his ongoing medication, routine check-ups with his gastroenterologist, and any treatment for future flare-ups.
- PMI Role: While David's initial diagnosis was covered, UC is classified as a chronic condition. His insurer will typically not cover ongoing medication, routine monitoring (e.g., annual colonoscopies for UC surveillance), or treatment for subsequent flare-ups, as these fall under the management of a chronic condition. This responsibility reverts to the NHS.
- Outcome: David must continue to receive his ongoing UC management, including medication and flare-up treatment, through the NHS. His private insurance only covered the initial acute phase of the new condition, demonstrating the 'acute care' focus of PMI.
These scenarios underscore the importance of understanding the precise definitions of 'acute', 'chronic', and 'pre-existing' within your policy.
Why a Broker Matters: Finding Your Best Fit with WeCovr
The UK private health insurance market is a complex landscape, with numerous insurers offering a vast array of policies, each with different levels of cover, excesses, exclusions, and underwriting terms. Trying to navigate this alone can be overwhelming, time-consuming, and potentially lead to a policy that doesn't meet your needs or expectations.
This is where an independent health insurance broker becomes an invaluable asset. A good broker acts as your expert guide, simplifying the process and helping you make an informed decision.
How an Independent Broker Helps:
- Market Expertise: Brokers have an in-depth understanding of the entire market, including the specific offerings, strengths, and weaknesses of each major insurer (e.g., Bupa, AXA Health, Vitality, Aviva, WPA, National Friendly, Freedom Health Insurance, The Exeter).
- Tailored Advice: Instead of a generic quote, a broker will take the time to understand your individual health needs, budget, existing medical history (crucial for digestive issues!), and preferences. They can then recommend policies that genuinely align with your requirements.
- Comparison Shopping: They can quickly compare multiple policies from various providers side-by-side, highlighting the key differences in cover, benefits, and exclusions that are relevant to your situation, especially concerning digestive health.
- Navigating Underwriting: Brokers are adept at explaining the nuances of full medical underwriting versus moratorium and can help you choose the best option based on your medical history, ensuring you understand the implications for any existing or potential future digestive issues.
- Clarifying the Small Print: Policy documents can be dense and confusing. A broker can break down complex terms, definitions (like 'acute' vs. 'chronic'), and exclusions, ensuring you fully comprehend what you're buying.
- Claims Guidance: While a broker doesn't process claims, they can often offer advice on the claims process and help you understand what information your insurer will require.
- Ongoing Support: Many brokers provide ongoing support throughout the life of your policy, assisting with renewals, changes to your circumstances, or general queries.
At WeCovr, we pride ourselves on being that guiding hand. We work with all major UK health insurers, comparing policies and explaining the nuances, ensuring you get the best possible cover for your specific needs, all at no additional cost to you. Our expert team at WeCovr understands the intricacies of underwriting and policy benefits, enabling us to navigate the market on your behalf. We're committed to transparency and clarity, ensuring you fully grasp how your policy will address your health concerns, particularly for complex areas like digestive health.
When you choose WeCovr, you're not just getting a quote; you're gaining a partner who understands the complexities of health insurance and is dedicated to finding you the most suitable and comprehensive protection, helping you achieve a fast track to peace of mind about your gut health.
The Future of Gut Health and Private Insurance
The field of digestive health is one of the most rapidly evolving areas of medicine. Research into the gut microbiome, personalised nutrition, and advanced diagnostic techniques is constantly expanding our understanding of how our gut influences every aspect of our health.
As our knowledge grows, it's plausible that private health insurance policies may adapt to reflect these advancements:
- More Integrated Wellness: Insurers might increasingly incorporate microbiome testing, advanced dietary advice, or even specific 'gut health' modules into their higher-tier wellness offerings.
- Personalised Medicine: As treatments become more tailored based on individual genetic or microbial profiles, policies might evolve to cover these more targeted therapies.
- Focus on Prevention: While traditionally focused on treatment, a greater emphasis on proactive gut health management through preventative screenings or lifestyle interventions might emerge as a value-add.
However, the core principle of private health insurance – covering acute, new conditions – is likely to remain. Chronic conditions will, for the foreseeable future, continue to be managed primarily through the NHS. Nonetheless, the ability of PMI to provide rapid diagnosis for new issues will remain invaluable as the complexity of gut health investigations continues to grow.
Taking the Next Step Towards Better Digestive Health
Living with digestive issues can be challenging, but access to timely and expert care can make a profound difference. UK private health insurance offers a valuable pathway to faster diagnosis and treatment for new and acute digestive conditions, helping to alleviate pain, reduce anxiety, and improve your quality of life.
While it's crucial to understand its limitations, particularly regarding pre-existing and chronic conditions, the benefits of expedited access to specialists, state-of-the-art diagnostics, and comfortable treatment environments are undeniable.
If you're considering private health insurance to support your digestive health, remember to:
- Assess your needs: What are your primary concerns and budget?
- Understand underwriting: Be clear on how your medical history will affect coverage.
- Read the policy documents: Pay close attention to definitions and exclusions.
- Utilise an expert broker: A broker can save you time, money, and stress by finding the best policy for your unique circumstances.
Don't let the complexities of the system deter you. Taking control of your health begins with informed choices. Explore your options for private health insurance today and empower yourself with the ability to fast track your journey to better gut health.
Invest in your health, and gain the peace of mind that comes with knowing you have direct access to leading digestive health experts when you need them most, for the acute conditions that life may throw your way.
Related guides
Why private medical insurance and how does it work?
What is Private Medical Insurance?
Private medical insurance (PMI) is a type of health insurance that provides access to private healthcare services in the UK. It covers the cost of private medical treatment, allowing you to bypass NHS waiting lists and receive faster, more convenient care.How does it work?
Private medical insurance works by paying for your private healthcare costs. When you need treatment, you can choose to go private and your insurance will cover the costs, subject to your policy terms and conditions. This can include:• Private consultations with specialists
• Private hospital treatment and surgery
• Diagnostic tests and scans
• Physiotherapy and rehabilitation
• Mental health treatment
Your premium depends on factors like your age, health, occupation, and the level of cover you choose. Most policies offer different levels of cover, from basic to comprehensive, allowing you to tailor the policy to your needs and budget.
Questions to ask yourself regarding private medical insurance
Just ask yourself:👉 Are you concerned about NHS waiting times for treatment?
👉 Would you prefer to choose your own consultant and hospital?
👉 Do you want faster access to diagnostic tests and scans?
👉 Would you like private hospital accommodation and better food?
👉 Do you want to avoid the stress of NHS waiting lists?
Many people don't realise that private medical insurance is more affordable than they think, especially when you consider the value of faster treatment and better facilities. A great insurance policy can provide peace of mind and ensure you receive the care you need when you need it.
Benefits offered by private medical insurance
Private medical insurance provides numerous benefits that can significantly improve your healthcare experience and outcomes:Faster Access to Treatment
One of the biggest advantages is avoiding NHS waiting lists. While the NHS provides excellent care, waiting times can be lengthy. With private medical insurance, you can often receive treatment within days or weeks rather than months.
Choice of Consultant and Hospital
You can choose your preferred consultant and hospital, giving you more control over your healthcare journey. This is particularly important for complex treatments where you want a specific specialist.
Better Facilities and Accommodation
Private hospitals typically offer superior facilities, including private rooms, better food, and more comfortable surroundings. This can make your recovery more pleasant and potentially faster.
Advanced Treatments
Private medical insurance often covers treatments and medications not available on the NHS, giving you access to the latest medical advances and technologies.
Mental Health Support
Many policies include comprehensive mental health coverage, providing faster access to therapy and psychiatric care when needed.
Tax Benefits for Business Owners
If you're self-employed or a business owner, private medical insurance premiums can be tax-deductible, making it a cost-effective way to protect your health and your business.
Peace of Mind
Knowing you have access to private healthcare when you need it provides invaluable peace of mind, especially for those with ongoing health conditions or concerns about NHS capacity.
Private medical insurance is particularly valuable for those who want to take control of their healthcare journey and ensure they receive the best possible treatment when they need it most.
Important Fact!
We can look at a more suitable option mid-term!
Why is it important to get private medical insurance early?
👉 Many people are very thankful that they had their private medical insurance cover in place before running into some serious health issues. Private medical insurance is as important as life insurance for protecting your family's finances.👉 We insure our cars, houses, and even our phones! Yet our health is the most precious thing we have.
Easily one of the most important insurance purchases an individual or family can make in their lifetime, the decision to buy private medical insurance can be made much simpler with the help of FCA-authorised advisers. They are the specialists who do the searching and analysis helping people choose between various types of private medical insurance policies available in the market, including different levels of cover and policy types most suitable to the client's individual circumstances.
It certainly won't do any harm if you speak with one of our experienced insurance experts who are passionate about advising people on financial matters related to private medical insurance and are keen to provide you with a free consultation.
You can discuss with them in detail what affordable private medical insurance plan for the necessary peace of mind they would recommend! WeCovr works with some of the best advisers in the market.
By tapping the button below, you can book a free call with them in less than 30 seconds right now:
Our Group Is Proud To Have Issued 900,000+ Policies!
We've established collaboration agreements with leading insurance groups to create tailored coverage
























How It Works
1. Complete a brief form

2. Our experts analyse your information and find you best quotes

3. Enjoy your protection!

Any questions?
Learn more

Who Are WeCovr?
WeCovr is an insurance specialist for people valuing their peace of mind and a great service.👍 WeCovr will help you get your private medical insurance, life insurance, critical illness insurance and others in no time thanks to our wonderful super-friendly experts ready to assist you every step of the way.
Just a quick and simple form and an easy conversation with one of our experts and your valuable insurance policy is in place for that needed peace of mind!