Beyond the First Symptom How UK Private Health Insurance Supports the Diagnostic Odyssey for Complex and Undiagnosed Conditions

Beyond the First Symptom: How UK Private Health Insurance Supports the Diagnostic Odyssey for Complex and Undiagnosed Conditions
Imagine a nagging ache that won't dissipate, a persistent fatigue that drains your energy, or a collection of seemingly unrelated symptoms that no one can quite piece together. For countless individuals across the UK, this isn't just a hypothetical scenario; it's the bewildering reality of living through a "diagnostic odyssey." This arduous journey is characterised by prolonged periods of uncertainty, countless appointments, and the emotional toll of not knowing what's truly wrong.
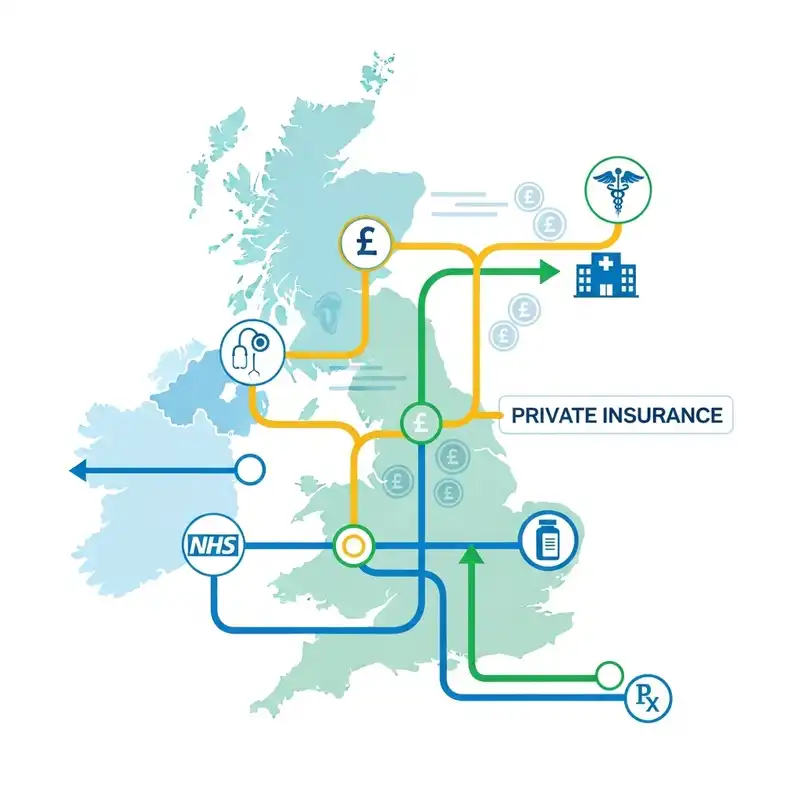
While our beloved NHS provides a phenomenal foundation for healthcare, its resources are finite, and the sheer volume of demand can sometimes mean that complex, atypical, or undiagnosed conditions present a significant challenge within its current structures. This is where UK private health insurance (PMI) often emerges not as a luxury, but as a critical enabler, offering a distinct pathway to accelerated investigation, expert opinions, and comprehensive diagnostic support.
This comprehensive guide will delve deep into the heart of the diagnostic odyssey, exploring how private health insurance can provide a vital lifeline when navigating the labyrinth of complex and undiagnosed health concerns. We'll demystify the process, highlight key benefits, and address common misconceptions, ensuring you understand how this valuable protection can empower you on your path to clarity and well-being.
Understanding the Diagnostic Odyssey: A Journey into the Unknown
The term "diagnostic odyssey" perfectly encapsulates the often-protracted and emotionally exhausting experience of trying to find a diagnosis for a persistent, complex, or unusual set of symptoms. It's a journey that can span months, even years, marked by numerous consultations, tests, and sometimes, the disheartening feeling of being misunderstood or dismissed.
What Defines an Odyssey?
- Elusive Symptoms: Symptoms that are vague, non-specific, or mimic many other conditions, making initial identification difficult. Examples include chronic fatigue, widespread pain, neurological oddities, or digestive disturbances that don't fit a clear pattern.
- Multi-system Involvement: Conditions that affect multiple bodily systems simultaneously, requiring input from various medical specialisms.
- Atypical Presentation: When a common condition presents in an unusual way, or when a rare condition is suspected but not immediately recognised.
- The "Rule-Out" Process: Doctors systematically eliminate common conditions, which is necessary but can be time-consuming and frustrating for the patient.
- Emotional and Psychological Burden: The constant uncertainty, anxiety, and frustration of not having a diagnosis can severely impact mental health, relationships, and daily life. Patients often feel isolated, unheard, and increasingly desperate for answers.
Why Do Diagnostic Odysseys Occur?
Several factors contribute to the complexity of these journeys:
- Rarity of Conditions: Many diseases are rare, meaning general practitioners and even some specialists may encounter them infrequently, if at all.
- Symptom Overlap: Numerous conditions share similar symptoms, making it difficult to differentiate them without advanced testing.
- Lack of Definitive Tests: For some conditions, there isn't one single, conclusive test. Diagnosis relies on a combination of clinical assessment, symptom patterns, and ruling out other possibilities.
- Fragmented Care: Without a central coordinating point, patients can find themselves bouncing between different specialists, each focusing on their own area, without a holistic view of the patient's overall health.
- Time and Resource Constraints: Within a busy healthcare system, the time available for thorough, multi-disciplinary investigation can be limited, especially for cases that don't fit standard diagnostic algorithms.
The diagnostic odyssey is not merely a medical challenge; it's a deeply personal one, impacting every facet of a patient's life. It underscores the profound need for efficient, comprehensive, and patient-centred diagnostic pathways.
The NHS and the Diagnostic Journey: Strengths and Strains
The National Health Service is a cornerstone of British society, providing universal healthcare regardless of ability to pay. It excels in delivering acute emergency care, managing chronic conditions, and performing complex surgeries on a vast scale. However, its very strengths can sometimes become areas of strain when confronted with the intricacies of a diagnostic odyssey.
Where the NHS Shines
- Universal Access: Everyone can access care, from GP appointments to specialist referrals.
- Emergency Care: World-class emergency services for life-threatening conditions.
- Chronic Disease Management: Robust systems for managing long-term conditions once diagnosed.
- Research and Innovation: A significant player in medical research and development.
The Pressures on the System
- Waiting Lists: Unprecedented demand often leads to significant waiting times for GP appointments, specialist consultations, and diagnostic tests. This can be particularly agonising when every passing week without answers feels like an eternity.
- Referral Pathways: The NHS typically operates on a hierarchical referral system. A GP refers to a general specialist, who may then refer to a sub-specialist. This sequential process, while necessary, can add considerable time to a diagnostic journey, especially for conditions requiring input from multiple, seemingly unrelated, disciplines.
- Resource Allocation: Finite budgets and staffing levels mean that access to the very latest diagnostic technologies or highly specialised consultants can be prioritised based on clinical urgency, potentially leaving those with complex, non-life-threatening, but profoundly debilitating, symptoms waiting.
- Holistic Overview: While efforts are made, truly integrated, multi-disciplinary team (MDT) approaches for diagnosis of complex, undifferentiated conditions can be challenging to coordinate swiftly across different NHS trusts and departments.
For someone embarking on a diagnostic odyssey, these systemic pressures can translate into extended periods of anxiety, worsening symptoms, and a delay in receiving appropriate treatment. This is not a failing of the dedicated NHS staff, but rather a reflection of a system under immense strain, particularly in areas requiring extensive, bespoke investigation.
How Private Health Insurance Steps In: Bridging the Gap
Private health insurance is designed to complement, not replace, the NHS. Its core value proposition lies in offering quicker access to private medical facilities, consultants, and advanced diagnostic tools. For individuals facing a diagnostic odyssey, this translates into several crucial advantages.
Core Benefits for Diagnostic Journeys:
-
Accelerated Access:
- Reduced Waiting Times: Perhaps the most immediate and tangible benefit. Instead of waiting weeks or months for an initial specialist appointment, you can often see a consultant privately within days. This rapid access can significantly compress the diagnostic timeline.
- Direct Specialist Access (via GP Referral): While you'll still typically need a referral from your GP (to ensure clinical necessity and guide the initial specialty), PMI often allows you to choose your consultant and hospital, or at least provides a list of immediately available experts. This can mean avoiding the general 'catch-all' specialist and going straight to the sub-specialist most likely to understand your nuanced symptoms.
-
Access to a Wider Pool of Experts:
- Consultant Choice: Many policies allow you to select your consultant from a network of approved specialists. This is invaluable when seeking an expert with a particular niche understanding of complex or rare conditions.
- Second Opinions: The ability to easily seek a second, or even third, opinion from a different consultant can be transformative. A fresh pair of eyes, a different line of questioning, or an alternative diagnostic approach can unlock answers where previous attempts have failed.
-
Advanced Diagnostic Capabilities:
- Cutting-Edge Technology: Private hospitals often have readily available access to state-of-the-art diagnostic imaging (such as advanced MRI, CT, and PET scans) and sophisticated laboratory tests.
- Timely Testing: Once a specialist recommends a test, private systems typically facilitate scheduling it much more quickly than in the public sector, avoiding further delays in the diagnostic process.
-
Integrated Care and Coordination:
- Multi-Disciplinary Approach: While the NHS does this, private care can sometimes offer a more fluid and rapid coordination between different specialists for complex cases, especially if you are seeing consultants within the same private hospital group. This can facilitate quicker cross-referrals and joint consultations.
- Personalised Attention: The private healthcare environment often allows for more extended consultation times, giving specialists more opportunity to delve into the nuances of your symptoms and medical history.
-
Comfort and Convenience:
- Private Rooms: While not directly diagnostic, the comfort of a private room during investigations or short admissions can reduce stress and aid recovery.
- Flexible Appointments: Greater flexibility in scheduling appointments around work and family commitments.
- Continuity of Care: Often, you will see the same consultant throughout your diagnostic journey, fostering a stronger doctor-patient relationship.
It’s important to clarify that while private health insurance significantly accelerates the diagnostic phase, the initial point of contact for any new health concern in the UK typically remains your NHS GP. Your GP plays a vital role in assessing your symptoms, providing an initial referral letter for private consultation, and integrating private findings back into your overall NHS record. This ensures a seamless continuum of care, regardless of which pathway you choose for diagnosis.
Key Pillars of PMI Support for Complex Cases
Delving deeper, let's explore the specific ways in which private health insurance underpins a more efficient and less stressful diagnostic journey for complex conditions.
1. Rapid Access to Specialists
The cornerstone of any effective diagnostic process is access to the right expert at the right time. For complex or undiagnosed conditions, this often means seeing a highly specialised consultant quickly.
- Beyond Generalists: Your GP is excellent at managing general health, but for obscure symptoms, a specialist in a particular field (e.g., a neurologist for unusual headaches, a rheumatologist for perplexing joint pain, or a gastroenterologist for chronic digestive issues) is crucial. PMI significantly shortens the wait to see these experts.
- Multiple Specialities: Sometimes, the diagnosis isn't straightforward and requires insights from several different specialisms. For example, a patient with fatigue, muscle weakness, and digestive problems might need to see a neurologist, an endocrinologist, and a gastroenterologist. Private health insurance facilitates concurrent or rapid sequential appointments with these various experts, avoiding lengthy waiting lists for each referral.
- Avoiding the "Referral Merry-Go-Round": In the public sector, you might be referred to a general consultant who then refers you to another, and so on. With PMI, once your GP has given you a referral, you can often directly access a sub-specialist (e.g., a neuro-immunologist instead of a general neurologist) if clinically appropriate, potentially cutting out several steps.
2. Advanced Diagnostic Imaging and Tests
Once with a specialist, the next critical step is often a series of diagnostic tests. The speed and availability of these tests are paramount in reaching a timely diagnosis.
- High-Tech Scans:
- MRI Scans: Crucial for detailed soft tissue imaging, identifying neurological conditions, joint issues, and abdominal problems.
- CT Scans: Excellent for bones, blood vessels, and detailed cross-sectional images of internal organs.
- PET Scans: Often used to detect cancers, inflammation, and neurological conditions by showing metabolic activity.
- Ultrasounds: Real-time imaging, useful for a wide range of conditions from abdominal to vascular. Private facilities typically have shorter waiting times for these high-demand scans.
- Specialised Laboratory Tests: Beyond routine blood tests, complex conditions often require highly specific blood markers, genetic tests, immunological panels, or advanced pathology. PMI covers these when deemed medically necessary by a specialist.
- Endoscopies and Biopsies: Procedures like gastroscopy, colonoscopy, or bronchoscopy, often accompanied by biopsies for tissue analysis, are fundamental for diagnosing many digestive, respiratory, and other internal conditions. Private access ensures these are performed promptly.
- Neurophysiology Tests: For neurological symptoms, tests like EMGs (electromyography) or nerve conduction studies can be vital for diagnosing conditions affecting nerves and muscles.
- Faster Results: Not only are the tests scheduled quicker, but the processing and reporting of results are often expedited in private settings, allowing for a quicker follow-up and diagnostic conclusion.
3. Second Opinions
When a diagnosis is elusive, or if you feel uncertain about a particular pathway, a second opinion can be invaluable.
- Fresh Perspective: A different consultant might approach your symptoms from an alternative angle, identify something previously overlooked, or suggest a different diagnostic pathway.
- Validation: Even if the second opinion confirms the first, it can provide immense peace of mind and confidence in the chosen diagnostic or treatment plan.
- Access to Specific Expertise: If your initial specialist admits they are at the limits of their expertise for your complex case, PMI facilitates access to another consultant known for their specific knowledge in rare or challenging conditions.
4. Mental Health Support
The diagnostic odyssey is not just physically draining; it's a profound psychological challenge. The uncertainty, frustration, and fear can lead to significant anxiety, depression, and stress.
- Integrated Support: Many PMI policies now include mental health benefits, covering consultations with psychiatrists, psychologists, and therapists.
- Early Intervention: Addressing the mental toll alongside the physical symptoms can be crucial. Prompt access to psychological support can help individuals cope with the uncertainty and stress of an undiagnosed illness, preventing further deterioration of mental well-being.
- Holistic Approach: Acknowledging and treating the psychological impact is part of a truly holistic approach to health.
5. Comfort and Convenience
While less directly related to diagnosis, the patient experience itself can significantly impact well-being during a stressful period.
- Private Hospital Environment: Often quieter, more comfortable, and offering a higher degree of privacy.
- Flexible Scheduling: More choice in appointment times to fit around work and family commitments, reducing disruption to daily life.
- Dedicated Patient Pathways: Some private hospitals offer dedicated navigators or patient liaison teams to help coordinate appointments and tests, simplifying the often-complex logistics of a multi-specialty diagnostic journey.
By providing these pillars of support, private health insurance empowers individuals to take a proactive role in their diagnostic journey, reducing wait times, expanding access to expertise, and ultimately, accelerating the path to diagnosis and appropriate care.
The Crucial Distinction: What PMI DOESN'T Cover
It is absolutely paramount to understand the limitations of private health insurance in the UK. Misconceptions in this area can lead to significant disappointment and financial strain. Private medical insurance primarily covers acute conditions, not chronic or pre-existing ones.
Let's break down these critical exclusions:
1. Pre-Existing Conditions
- Definition: A pre-existing condition is any disease, illness, or injury for which you have received medication, advice, or treatment, or had symptoms, before your private health insurance policy started.
- Why They're Excluded: Insurers assess risk. If they covered conditions you already had symptoms for, or were diagnosed with before taking out the policy, it would be akin to trying to insure your car after you've had an accident.
- Impact on Diagnostic Odyssey: This is a crucial point for diagnostic odysseys. If you started experiencing vague symptoms before you took out the policy, and these symptoms ultimately lead to a diagnosis, that diagnosis (and any subsequent treatment) may be excluded.
- Example: You experience unexplained fatigue and joint pain for six months, then take out PMI. Two months later, you see a private rheumatologist via your new policy, and they diagnose you with an autoimmune condition. The insurer may decline coverage, as the symptoms pre-dated the policy start.
- Underwriting Methods: Insurers use different methods to assess pre-existing conditions:
- Full Medical Underwriting: You provide your full medical history upfront. The insurer will then list any exclusions specifically on your policy. This offers clarity from the outset.
- Moratorium Underwriting: You don't declare your full history initially. Instead, the insurer automatically excludes any condition for which you've had symptoms, advice, or treatment in a set period (e.g., the last five years). If you go symptom-free for a continuous period (e.g., two years) after taking out the policy, that condition may then become covered. This method is common but requires careful understanding, especially for undiagnosed symptoms that might later be linked to a pre-existing issue.
It is vital to be completely honest about your medical history when applying for PMI, as any non-disclosure could invalidate your policy.
2. Chronic Conditions
- Definition: A chronic condition is a disease, illness, or injury that has one or more of the following characteristics:
- It continues indefinitely.
- It has no known cure.
- It requires long-term monitoring, control, or relief of symptoms.
- It requires rehabilitation.
- It requires special training of the patient to cope with its effects.
- Why They're Excluded: PMI is designed for acute conditions – those that respond quickly to treatment and enable you to return to full health. Chronic conditions require ongoing, long-term management, which falls outside the scope of what most PMI policies are designed to cover.
- Impact on Diagnostic Odyssey: PMI can cover the diagnostic phase of a chronic condition. So, if you develop new symptoms and through private means are diagnosed with, say, Type 1 Diabetes (a chronic condition), the investigations leading to that diagnosis would typically be covered (assuming the symptoms didn't pre-date the policy). However, once diagnosed, the ongoing management, medication, monitoring, and treatment for the diabetes itself would then fall back to the NHS.
- Example: You develop new, persistent digestive issues. Your PMI covers all the tests (endoscopies, biopsies, scans) that lead to a diagnosis of Crohn's disease (a chronic condition). The diagnostic costs are covered. Once diagnosed, however, the ongoing medication, regular consultant follow-ups, and any future flare-up management for Crohn's would typically be managed by the NHS.
- Distinction between Acute and Chronic: This distinction is key. PMI is there to help get you diagnosed and treated for an acute issue, or to get a diagnosis for a chronic one. It is not there to fund the lifetime management of a chronic illness.
Other Common Exclusions:
- Routine Pregnancy and Childbirth: Complications can sometimes be covered, but routine care is not.
- Cosmetic Surgery: Unless medically necessary following an accident or illness.
- Fertility Treatment: Generally excluded.
- Emergency A&E Treatment: Private hospitals usually don't have A&E departments equipped for major emergencies. You'd go to the NHS.
- Drug and Alcohol Abuse: Treatment for addiction is typically not covered.
- Overseas Treatment: Most policies cover treatment within the UK only.
- Self-inflicted Injuries: Not covered.
- Organ Transplants: Usually not covered as part of standard policies.
- HIV/AIDS: Specific exclusions often apply.
Understanding these exclusions is paramount when considering private health insurance, particularly when thinking about its role in complex or undiagnosed conditions. It's about getting answers quickly, and potentially treating acute conditions, not about bypassing the NHS for long-term chronic care or pre-existing ailments. Always read your policy documents carefully, and if in doubt, ask your insurer or broker for clarification.
Navigating the Policy: Understanding Your Coverage
Once you’ve decided to explore private health insurance, deciphering the various terms and benefits can feel overwhelming. Knowing what your policy covers and the associated limits is critical, especially when dealing with complex diagnostic pathways.
Key Terms and Benefits to Understand:
-
In-Patient, Out-Patient, and Day-Patient Benefits:
- In-Patient: Covers treatment received when formally admitted to a hospital bed overnight. This includes surgery, hospital accommodation, nursing care, and consultants' fees.
- Day-Patient: Covers treatment received when admitted to a hospital bed for a day but not staying overnight (e.g., for a minor procedure or extensive diagnostics).
- Out-Patient: Covers consultations with specialists, diagnostic tests (like blood tests, X-rays, MRI scans), and sometimes physiotherapy or other therapies, where you are not formally admitted to a hospital bed.
- Importance for Diagnostic Odysseys: For undiagnosed conditions, out-patient limits are crucial. The initial phase often involves multiple specialist consultations and extensive diagnostic tests (scans, blood tests, biopsies) – all typically falling under outpatient benefits. Some policies have generous outpatient limits, while others have very restricted ones, or even no outpatient cover at all unless it leads to an inpatient admission. Ensure your policy has sufficient outpatient cover for the diagnostic phase.
-
Excess:
- This is the amount you agree to pay towards the cost of your claim. For example, if you have a £250 excess, you pay the first £250 of your claim, and the insurer pays the rest (up to your policy limits).
- A higher excess usually results in lower premiums. Consider whether you’re comfortable paying this amount if you need to make a claim.
-
Co-Payments/Co-Insurance:
- Some policies might require you to pay a percentage of the total cost of treatment, in addition to an excess. For example, you might pay 10% of the claim, with the insurer paying 90%. This is less common in the UK compared to some other countries but can exist.
-
Policy Limits:
- Monetary Limits: Policies often have overall annual monetary limits (e.g., £1 million per year) or specific limits for certain benefits (e.g., £1,000 for outpatient consultations, £500 for physiotherapy). For a diagnostic odyssey involving numerous tests and consultations, ensuring these limits are adequate is vital.
- Session Limits: Some benefits, particularly for therapies like physiotherapy or mental health support, might have limits on the number of sessions allowed per condition or per year.
-
Open Referral vs. Named Consultant:
- Most policies require a GP referral. The referral can be "open" (referring you to a specialist in a particular field, allowing the insurer to suggest a consultant within their network) or "named" (your GP specifically refers you to a consultant by name).
- Having the flexibility to choose a named consultant, especially for rare or complex conditions, can be beneficial, but some policies might restrict this or offer it only on higher-tier plans.
-
Hospital Networks:
- Insurers work with a network of private hospitals. Some policies offer access to all private hospitals (including premium central London hospitals), while others might have a more restricted list. Your premium will vary based on the network you choose.
- Consider whether the hospitals in your chosen network are convenient for you and if they have the specific facilities or specialists you might need.
-
Underwriting Method:
- As discussed earlier, understanding whether your policy is on a Full Medical Underwriting or Moratorium basis is critical, especially regarding potential pre-existing conditions and their impact on future claims for undiagnosed symptoms.
Reading Your Policy Documents:
The policy document, often called a "Policy Wording" or "Terms and Conditions," is the definitive source of truth for your coverage. It's often lengthy and filled with legal jargon, but it's essential reading. Pay particular attention to:
- Exclusions Section: A detailed list of what is not covered.
- Benefits Schedule: A clear breakdown of what is covered, with any limits applied.
- Claims Process: How to initiate a claim, what documentation is required, and what approvals you need.
Navigating this complexity can be daunting, which is where independent advice becomes invaluable.
The Role of Your GP: Still Your First Port of Call
Despite the perceived "faster access" of private health insurance, your NHS GP remains an absolutely vital part of your healthcare journey in the UK, even when you have PMI. They are not bypassed; rather, they form the crucial bridge between public and private care.
Your GP's Essential Functions:
-
Initial Assessment and Triage:
- Your GP is the expert in general medicine. They are your first point of contact for any new symptoms or health concerns. They will conduct an initial assessment, take your full medical history, perform preliminary examinations, and order basic tests if necessary.
- Their role is to rule out common conditions and identify if your symptoms warrant specialist investigation.
-
The Referral Gateway:
- For almost all private health insurance claims, you will require a referral letter from your GP to a private consultant. This letter is not just a formality; it serves several critical purposes:
- Clinical Justification: It provides the private consultant (and your insurer) with a summary of your symptoms, medical history, and why a specialist opinion is needed. This demonstrates clinical necessity for the private investigation.
- Direction: Your GP can guide you towards the most appropriate specialist based on your symptoms (e.g., neurologist, rheumatologist, gastroenterologist).
- Insurance Requirement: Insurers generally will not authorise a private consultation or treatment without a GP referral.
- For almost all private health insurance claims, you will require a referral letter from your GP to a private consultant. This letter is not just a formality; it serves several critical purposes:
-
Coordination of Care:
- Even when you are undergoing private diagnostic tests or seeing a private specialist, your GP should remain informed.
- They act as your central medical record keeper, receiving reports back from private consultants and tests. This ensures your overall health record is cohesive and that any private findings are integrated into your ongoing care plan, whether that care continues privately or transitions back to the NHS.
- This coordination is especially important for complex or undiagnosed conditions where multiple specialists might be involved. Your GP is best placed to hold the complete picture.
-
Ongoing Care Management:
- If your private diagnostic journey leads to a diagnosis that requires long-term management (e.g., a chronic condition), your GP will typically resume responsibility for your ongoing care within the NHS. As discussed, PMI usually covers the diagnosis but not the long-term management of chronic illnesses.
-
Emergency Management:
- For acute emergencies (e.g., sudden severe chest pain, stroke symptoms, major accidents), your GP will direct you to an NHS A&E department, as private hospitals generally do not have the same level of emergency care facilities.
In essence, your GP remains your healthcare anchor. Private health insurance simply provides an alternative, accelerated pathway for specialist consultations and diagnostics, working in partnership with your GP to get you the answers you need more quickly. Building a strong, trusting relationship with your GP is therefore just as important for private patients as it is for those who rely solely on the NHS.
Real-Life Scenarios: How PMI Can Make a Difference
Let's illustrate the value of private health insurance in the context of a diagnostic odyssey with a few hypothetical, yet common, scenarios.
Scenario 1: The Case of Persistent Fatigue and Neurological Symptoms
Patient: Sarah, 38, previously healthy. Symptoms: Over six months, Sarah develops increasing fatigue, intermittent numbness and tingling in her limbs, brain fog, and occasional blurry vision. Her NHS GP conducts standard blood tests, which come back normal. The GP suspects something neurological but warns of a 4-6 month waiting list for an NHS neurology consultation and a further wait for an MRI.
The Diagnostic Odyssey without PMI: Sarah experiences worsening symptoms, impacting her work and family life. The long wait for an NHS neurologist is anxiety-inducing. During this time, her symptoms fluctuate, making her doubt herself. Once she sees the neurologist, further delays for an MRI and subsequent follow-up mean a diagnosis could take over a year from the onset of symptoms.
The Diagnostic Odyssey with PMI:
- GP Referral: Sarah sees her NHS GP, who provides a referral letter to a private neurologist.
- Rapid Private Consultation: Within days, Sarah has an appointment with a leading private neurologist. The neurologist takes a detailed history and, based on her symptoms, immediately suspects a demyelinating condition like Multiple Sclerosis.
- Expedited Diagnostics: The neurologist refers Sarah for an urgent brain and spinal MRI scan, which she undergoes within the week at a private imaging centre. The results are back within 48 hours.
- Swift Diagnosis & Initial Treatment Plan: The MRI confirms lesions consistent with MS. The neurologist explains the diagnosis, discusses initial treatment options, and refers her to an MS nurse.
- Transition to NHS for Chronic Management: While the diagnosis was covered by PMI, ongoing treatment, medication, and long-term management for MS (a chronic condition) transition back to the NHS, where Sarah is now connected to specialist services quickly due to her confirmed diagnosis.
Benefit of PMI: Sarah receives a diagnosis and begins treatment within weeks of her private consultation, rather than months or a year later. This significantly reduces her distress and allows for earlier intervention, which can improve long-term outcomes for conditions like MS.
Scenario 2: Chronic Digestive Issues and Unexplained Weight Loss
Patient: David, 55, active and health-conscious. Symptoms: For eight months, David has suffered from chronic abdominal pain, bloating, unpredictable bowel habits (alternating between constipation and diarrhoea), and has lost a significant amount of weight unintentionally. His NHS GP has tried dietary changes and initial medications, but without success. Referral to an NHS gastroenterologist is estimated at 3-4 months.
The Diagnostic Odyssey without PMI: David's symptoms continue to severely impact his quality of life, making socialising and work challenging. The wait for a specialist causes increasing anxiety, especially given the weight loss which raises cancer concerns. He might try various restrictive diets without proper guidance, leading to nutritional deficiencies.
The Diagnostic Odyssey with PMI:
- GP Referral: David's NHS GP refers him to a private gastroenterologist, highlighting the weight loss and persistent symptoms.
- Quick Specialist Access: David sees a private gastroenterologist within a week. The specialist listens thoroughly to his symptoms and orders a comprehensive diagnostic workup.
- Comprehensive Diagnostics: Within two weeks, David undergoes:
- A full set of specialised blood tests (including inflammatory markers, coeliac screen, and stool tests).
- An urgent colonoscopy and gastroscopy with biopsies.
- An abdominal MRI scan.
- Timely Diagnosis and Path Forward: The results indicate Crohn's disease (a chronic inflammatory bowel condition). While Crohn's is chronic, the diagnostic process was fully covered. The private gastroenterologist provides immediate guidance on diet, lifestyle, and initial medication options.
- NHS Handover for Management: David is then referred back to the NHS, with a clear diagnosis and recommended treatment plan, enabling a much smoother and faster transition into NHS specialist inflammatory bowel disease (IBD) clinics for ongoing management.
Benefit of PMI: David avoids prolonged suffering and anxiety. The comprehensive and rapid diagnostic tests allow for a definitive diagnosis of a potentially serious condition, enabling immediate implementation of a management strategy.
Scenario 3: The Enigma of Widespread Pain and Fatigue
Patient: Lisa, 45, professional with a busy family life. Symptoms: Lisa has been experiencing widespread muscular pain, joint stiffness, profound fatigue, and sleep disturbances for over a year. Her NHS GP has ruled out common conditions like thyroid issues and vitamin deficiencies. Suspecting a more complex rheumatological condition or chronic pain syndrome, the NHS waiting list for a rheumatologist is lengthy.
The Diagnostic Odyssey without PMI: Lisa's quality of life deteriorates significantly. The pain and fatigue make it difficult to work and care for her children. The lack of a diagnosis exacerbates feelings of frustration and despair. She might be offered symptomatic management without understanding the root cause.
The Diagnostic Odyssey with PMI:
- GP Referral: Lisa's GP provides a referral to a private rheumatologist.
- Specialist Consultation and Initial Assessment: Lisa sees a private rheumatologist within days. The rheumatologist conducts a thorough physical examination and orders a series of advanced immunological blood tests.
- Multi-Disciplinary Input: The initial tests are inconclusive but point towards a complex pain disorder. The rheumatologist, suspecting fibromyalgia or a related condition, might refer her for further assessment with a pain management specialist or recommend a session with a clinical psychologist (if covered by her policy for diagnostic purposes or initial assessment).
- Holistic Diagnostic Approach: Through a combination of further clinical assessment, exclusion of other conditions, and a multi-disciplinary perspective, the private team helps Lisa reach a working diagnosis of fibromyalgia.
- Guided Self-Management and NHS Link: The private rheumatologist provides a comprehensive management plan, including recommendations for physiotherapy, occupational therapy, and pain management strategies (some of which may be covered for a short period by her policy if they are part of the acute phase of diagnosis and initial treatment). Lisa is then guided on how to access ongoing support and chronic pain management services through the NHS, armed with a clear diagnosis.
Benefit of PMI: Lisa receives a diagnosis for a condition that is often difficult to pinpoint. The rapid and integrated approach of the private system provides clarity and a structured plan for managing her symptoms, significantly improving her well-being and empowering her to cope.
These examples underscore that private health insurance is not about bypassing the NHS entirely but about accelerating access to specialist expertise and advanced diagnostics when time is of the essence and the path to diagnosis is unclear.
Choosing the Right Policy: A Strategic Approach
Selecting the right private health insurance policy is not a one-size-fits-all decision, especially when considering its potential role in complex diagnostic journeys. A strategic approach will ensure you get the most appropriate cover for your needs.
Key Considerations When Choosing a Policy:
-
Assess Your Needs and Risk Factors:
- Family Medical History: Are there any complex or chronic conditions in your family history that might inform your coverage needs? (Remember, pre-existing conditions won't be covered, but awareness helps in planning).
- Lifestyle: Do you lead a high-stress lifestyle? Are there any health concerns that are becoming persistent?
- Desired Level of Control: How important is it for you to choose your consultant or hospital?
- Budget: What can you realistically afford in premiums and excesses?
-
Understand Different Policy Types:
- Comprehensive Policies: Offer the broadest range of cover, including extensive outpatient benefits, mental health support, and wide hospital networks. These are often the most suitable for complex diagnostic odysseys due to their high outpatient limits.
- Mid-Range Policies: May offer good inpatient and day-patient cover but might have lower outpatient limits or restricted hospital networks.
- Basic/Budget Policies: Primarily cover inpatient treatment only, with very limited or no outpatient cover. These are generally not suitable for complex diagnostic journeys, as most of the initial investigation (consultations, scans, tests) happens on an outpatient basis.
-
Scrutinise Outpatient Benefits:
- As highlighted earlier, the diagnostic phase for complex and undiagnosed conditions relies heavily on outpatient consultations and tests. Ensure the policy you choose has robust outpatient cover – either an unlimited amount or a sufficiently high monetary limit (e.g., £1,000, £2,000, or more per year).
-
Check Hospital Networks:
- Does the insurer's network include private hospitals that are convenient for you and, crucially, known for having specialists in the areas you might anticipate needing? Some central London hospitals, for instance, are very expensive and are only included in premium policies.
-
Evaluate Underwriting Methods:
- Decide between Full Medical Underwriting (more upfront clarity on exclusions) and Moratorium (simpler application, but requires a symptom-free period for pre-existing conditions to become covered). If you have any current unexplained symptoms, full medical underwriting often provides more certainty from day one.
-
Consider Additional Benefits:
- Mental Health Support: Given the psychological toll of a diagnostic odyssey, comprehensive mental health benefits are a significant plus.
- Therapies: Does the policy cover physiotherapy, osteopathy, or chiropractic treatment if recommended by a specialist during your diagnostic phase or for acute issues?
- Virtual GP Services: Many policies now offer 24/7 virtual GP access, which can be a convenient first step for advice or initial referrals.
-
The Value of Independent Advice:
- The private health insurance market in the UK is diverse, with numerous insurers (e.g., Bupa, AXA Health, Vitality, Aviva, WPA, National Friendly, Freedom Health, etc.) offering a multitude of plans. Comparing policies directly can be time-consuming and confusing. This is where an independent health insurance broker comes in.
How WeCovr Can Help You Navigate This Complexity
At WeCovr, we understand the intricacies of the UK private health insurance market and the unique challenges faced by individuals on a diagnostic odyssey. Our mission is to simplify this complex landscape for you, ensuring you find the best possible cover without any hassle or cost.
Our Approach:
- Independent and Unbiased: We are an independent UK health insurance broker. This means we are not tied to any single insurer. We work with all major UK private health insurance providers, including Bupa, AXA Health, Vitality, Aviva, WPA, and many others. Our advice is always impartial, focused solely on your best interests.
- Access to the Entire Market: We have access to the full range of policies available, from comprehensive plans to more tailored options. This breadth of choice is crucial because what suits one person for a diagnostic odyssey might not suit another.
- Personalised Advice: We take the time to understand your individual health needs, your budget, your family history, and any specific concerns you might have. We listen to your potential diagnostic concerns and advise on policies that offer the most robust outpatient and diagnostic benefits.
- Policy Comparison and Simplification: We do the legwork for you. We compare multiple quotes from different insurers, highlight key differences in benefits, limits, excesses, and exclusions, and explain everything in clear, jargon-free language. We help you understand the small print so there are no surprises.
- Cost-Free Service: Our service to you is entirely free. We are paid a commission by the insurer if you decide to take out a policy through us, but this does not affect the premium you pay. You pay exactly the same, if not less (due to our ability to secure preferential rates), than if you went direct to the insurer.
- Ongoing Support: Our relationship doesn't end once your policy is in place. We are here to answer your questions, help you understand your policy at renewal, and provide support if you need to make a claim. We understand that navigating a diagnostic journey can be stressful, and we aim to be a supportive partner throughout.
Choosing the right private health insurance is an investment in your peace of mind and your health. For complex and undiagnosed conditions, it can mean the difference between months or years of uncertainty and a swift path to diagnosis and appropriate care. Let us help you find the perfect fit.
The Investment in Your Health: Beyond the Financial Cost
When considering private health insurance, it's natural to focus on the premiums. However, for those facing the daunting prospect of a diagnostic odyssey, the value of PMI extends far beyond monetary terms. It represents an investment in something far more profound: your well-being, your peace of mind, and ultimately, your future.
The True Value Proposition:
- Reduced Anxiety and Stress: The mental toll of living with undiagnosed symptoms and facing long waiting lists is immense. Knowing you have access to prompt consultations and rapid diagnostics can significantly alleviate this psychological burden. The peace of mind that comes from knowing you are actively pursuing answers is invaluable.
- Timely Intervention: For many conditions, early diagnosis can lead to more effective treatment, better long-term outcomes, and in some cases, can prevent the progression of a disease to a more severe stage. This is particularly true for conditions like autoimmune diseases, neurological disorders, or certain cancers, where every week counts.
- Preservation of Quality of Life: Protracted diagnostic delays can severely impact your ability to work, engage in hobbies, and maintain relationships. By accelerating the diagnostic process, PMI helps you return to a better quality of life sooner, reducing the cumulative impact of illness on your daily existence.
- Empowerment: Taking out private health insurance can be an act of empowerment. It puts you in a position to be proactive about your health, giving you choices and control over your healthcare journey when you might otherwise feel helpless.
- Complementary Care, Not Competition: PMI works hand-in-hand with the NHS. It takes pressure off the public system for complex diagnostic cases while ensuring you get the swift answers you need. Once a diagnosis is made, especially for chronic conditions, the NHS stands ready to provide ongoing management. This collaboration strengthens the overall healthcare landscape.
- Access to Niche Expertise: For rare or extremely complex conditions, being able to access a specific, highly specialised consultant who may not be easily accessible within the NHS's regional structure can be a game-changer.
While the financial outlay for premiums is a consideration, weigh it against the potential costs of delayed diagnosis: lost income, increased stress, progression of illness, and the sheer mental and emotional exhaustion. For many, the ability to shorten a diagnostic odyssey makes private health insurance an investment that truly pays dividends in health and happiness.
Conclusion
The diagnostic odyssey for complex and undiagnosed conditions is a challenging path, often fraught with uncertainty, frustration, and significant emotional strain. While the NHS remains a foundational pillar of UK healthcare, its inherent pressures can prolong this journey, delaying vital answers and subsequent treatment.
Private health insurance emerges as a powerful tool to navigate this labyrinth more effectively. By offering rapid access to specialists, cutting-edge diagnostic tests, opportunities for second opinions, and essential mental health support, PMI can significantly compress the diagnostic timeline. It transforms a prolonged wait into a focused, accelerated search for clarity, empowering individuals to take control of their health journey.
It is crucial, however, to approach private health insurance with a clear understanding of its scope – specifically, its focus on acute conditions and its necessary exclusion of pre-existing and chronic conditions for ongoing management. Used strategically, in partnership with your NHS GP, it complements the public system, providing a robust pathway to diagnosis when time and expertise are of the essence.
At WeCovr, we believe that everyone deserves clarity and peace of mind when it comes to their health. We are dedicated to helping you find a private health insurance policy that perfectly aligns with your needs, ensuring that should you ever embark on a diagnostic odyssey, you do so with the best possible support behind you. Don't let uncertainty define your health journey. Explore your options today and take the first step towards a clearer path.
Related guides
Why private medical insurance and how does it work?
What is Private Medical Insurance?
Private medical insurance (PMI) is a type of health insurance that provides access to private healthcare services in the UK. It covers the cost of private medical treatment, allowing you to bypass NHS waiting lists and receive faster, more convenient care.How does it work?
Private medical insurance works by paying for your private healthcare costs. When you need treatment, you can choose to go private and your insurance will cover the costs, subject to your policy terms and conditions. This can include:• Private consultations with specialists
• Private hospital treatment and surgery
• Diagnostic tests and scans
• Physiotherapy and rehabilitation
• Mental health treatment
Your premium depends on factors like your age, health, occupation, and the level of cover you choose. Most policies offer different levels of cover, from basic to comprehensive, allowing you to tailor the policy to your needs and budget.
Questions to ask yourself regarding private medical insurance
Just ask yourself:👉 Are you concerned about NHS waiting times for treatment?
👉 Would you prefer to choose your own consultant and hospital?
👉 Do you want faster access to diagnostic tests and scans?
👉 Would you like private hospital accommodation and better food?
👉 Do you want to avoid the stress of NHS waiting lists?
Many people don't realise that private medical insurance is more affordable than they think, especially when you consider the value of faster treatment and better facilities. A great insurance policy can provide peace of mind and ensure you receive the care you need when you need it.
Benefits offered by private medical insurance
Private medical insurance provides numerous benefits that can significantly improve your healthcare experience and outcomes:Faster Access to Treatment
One of the biggest advantages is avoiding NHS waiting lists. While the NHS provides excellent care, waiting times can be lengthy. With private medical insurance, you can often receive treatment within days or weeks rather than months.
Choice of Consultant and Hospital
You can choose your preferred consultant and hospital, giving you more control over your healthcare journey. This is particularly important for complex treatments where you want a specific specialist.
Better Facilities and Accommodation
Private hospitals typically offer superior facilities, including private rooms, better food, and more comfortable surroundings. This can make your recovery more pleasant and potentially faster.
Advanced Treatments
Private medical insurance often covers treatments and medications not available on the NHS, giving you access to the latest medical advances and technologies.
Mental Health Support
Many policies include comprehensive mental health coverage, providing faster access to therapy and psychiatric care when needed.
Tax Benefits for Business Owners
If you're self-employed or a business owner, private medical insurance premiums can be tax-deductible, making it a cost-effective way to protect your health and your business.
Peace of Mind
Knowing you have access to private healthcare when you need it provides invaluable peace of mind, especially for those with ongoing health conditions or concerns about NHS capacity.
Private medical insurance is particularly valuable for those who want to take control of their healthcare journey and ensure they receive the best possible treatment when they need it most.
Important Fact!
We can look at a more suitable option mid-term!
Why is it important to get private medical insurance early?
👉 Many people are very thankful that they had their private medical insurance cover in place before running into some serious health issues. Private medical insurance is as important as life insurance for protecting your family's finances.👉 We insure our cars, houses, and even our phones! Yet our health is the most precious thing we have.
Easily one of the most important insurance purchases an individual or family can make in their lifetime, the decision to buy private medical insurance can be made much simpler with the help of FCA-authorised advisers. They are the specialists who do the searching and analysis helping people choose between various types of private medical insurance policies available in the market, including different levels of cover and policy types most suitable to the client's individual circumstances.
It certainly won't do any harm if you speak with one of our experienced insurance experts who are passionate about advising people on financial matters related to private medical insurance and are keen to provide you with a free consultation.
You can discuss with them in detail what affordable private medical insurance plan for the necessary peace of mind they would recommend! WeCovr works with some of the best advisers in the market.
By tapping the button below, you can book a free call with them in less than 30 seconds right now:
Our Group Is Proud To Have Issued 900,000+ Policies!
We've established collaboration agreements with leading insurance groups to create tailored coverage
























How It Works
1. Complete a brief form

2. Our experts analyse your information and find you best quotes

3. Enjoy your protection!

Any questions?
Learn more

Who Are WeCovr?
WeCovr is an insurance specialist for people valuing their peace of mind and a great service.👍 WeCovr will help you get your private medical insurance, life insurance, critical illness insurance and others in no time thanks to our wonderful super-friendly experts ready to assist you every step of the way.
Just a quick and simple form and an easy conversation with one of our experts and your valuable insurance policy is in place for that needed peace of mind!